The challenges of detoxification for inmates in correctional facilities are becoming increasingly evident. Many individuals enter jails with severe medical and mental health conditions, putting their well-being at risk during the detox process. This concern was highlighted during a recent tour of the Sangamon County Jail in Springfield, Illinois, led by Superintendent Larry Beck in November 2023. Beck noted that the jail staff is striving to meet the growing demand for care among these inmates.
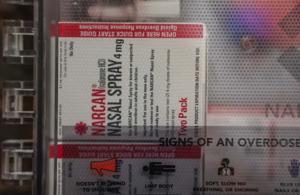
Correctional facilities like McLean County Jail have implemented measures to address opioid overdoses, including the use of Narcan kits to reverse overdose symptoms. Meanwhile, the Macon County Jail previously offered a Restore program aimed at helping inmates transition back into society. However, staff shortages have hindered the continuation of such initiatives in recent years.
The stigma surrounding substance use disorders and mental health conditions affects how these issues are perceived and treated. Research indicates that substance use disorders often co-occur with mental health conditions, complicating both diagnosis and treatment. These disorders are typically characterized by an inability to control substance use, impacting individuals’ daily lives.
In 2020, approximately 6.7% of U.S. adults—around 17 million people—were diagnosed with both a substance use disorder and at least one other mental illness. Notably, individuals with serious mental illnesses showed significantly higher rates of co-occurring substance use disorders. For instance, misuse of opioids and tranquilizers was roughly 6 percentage points higher among those with serious mental illnesses compared to those without.
Understanding the interplay between these conditions is crucial. Substance use disorders are recognized as mental health conditions influenced by various factors, including genetics, trauma, and environmental conditions. Acknowledging this connection is vital for reducing stigma and improving access to treatment.
According to data from the Substance Abuse and Mental Health Services Administration, more than half of all U.S. adults will receive a mental illness diagnosis in their lifetime. Common mental health conditions include depression, anxiety, and post-traumatic stress disorder, many of which frequently coexist with substance use disorders.
The relationship between genetics and mental health has become clearer in recent decades. Studies suggest that while no single gene is responsible for mental disorders, numerous gene variants can influence susceptibility. Genetics account for 40% to 60% of an individual’s risk for developing a substance use disorder, highlighting the importance of family history in understanding these conditions.
Environmental factors, particularly traumatic experiences, also play a significant role. Such experiences can alter brain function and even trigger genetic changes, leading to mental health or substance use disorders. This phenomenon, known as epigenetics, illustrates how external circumstances can impact internal health.
Furthermore, individuals experiencing psychological distress may resort to self-medication with psychoactive substances, increasing their risk of developing both mental health conditions and substance use disorders. The use of these substances can trigger symptoms similar to those of mental illnesses, complicating diagnosis and treatment.
Integrated treatments that address both substance use disorders and mental health conditions simultaneously are considered the most effective. They recognize the interconnected nature of these issues, allowing for comprehensive care. Despite this, significant barriers remain to accessing treatment. Stigma associated with both conditions can deter individuals from seeking help, as they fear potential repercussions such as job loss or social ostracism.
Financial barriers also contribute to disparities in access to quality care. Data shows stark differences in treatment access along racial and socioeconomic lines. For example, 37.6% of white adults needing treatment received care, compared to only 22.4% of Latino adults and 25% of Black Americans.
Efforts to destigmatize mental health and substance use disorders, coupled with improved access to treatment, are crucial for ensuring that individuals receive the support they need. As the conversation surrounding these issues evolves, it is essential to continue addressing the needs of vulnerable populations, particularly those within the correctional system.
This story originally appeared on Zinnia Health and was produced and distributed in partnership with Stacker Studio.