UPDATE: Stanford scientists have just revealed critical findings on how mRNA COVID-19 vaccines can, in rare cases, trigger heart inflammation, particularly in young men. Their groundbreaking study, published on December 10, 2025, uncovers the biological mechanisms behind this rare side effect and highlights potential strategies to mitigate the risks.
Researchers at Stanford Medicine have identified a two-step immune response linked to mRNA vaccines that floods the body with inflammatory signals. This response draws aggressive immune cells into the heart, leading to temporary injury, especially in adolescent and young adult males. The study emphasizes the importance of understanding these mechanisms to enhance vaccine safety while maintaining their effectiveness.
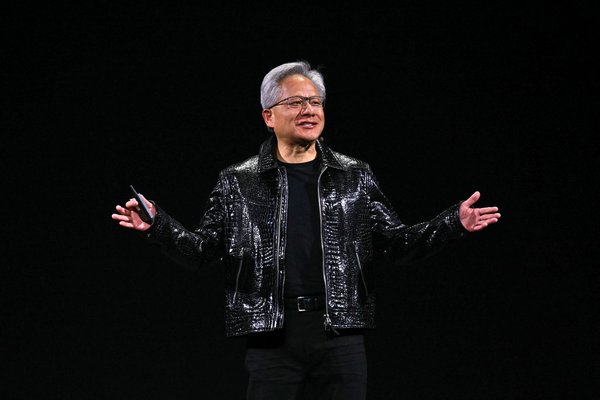
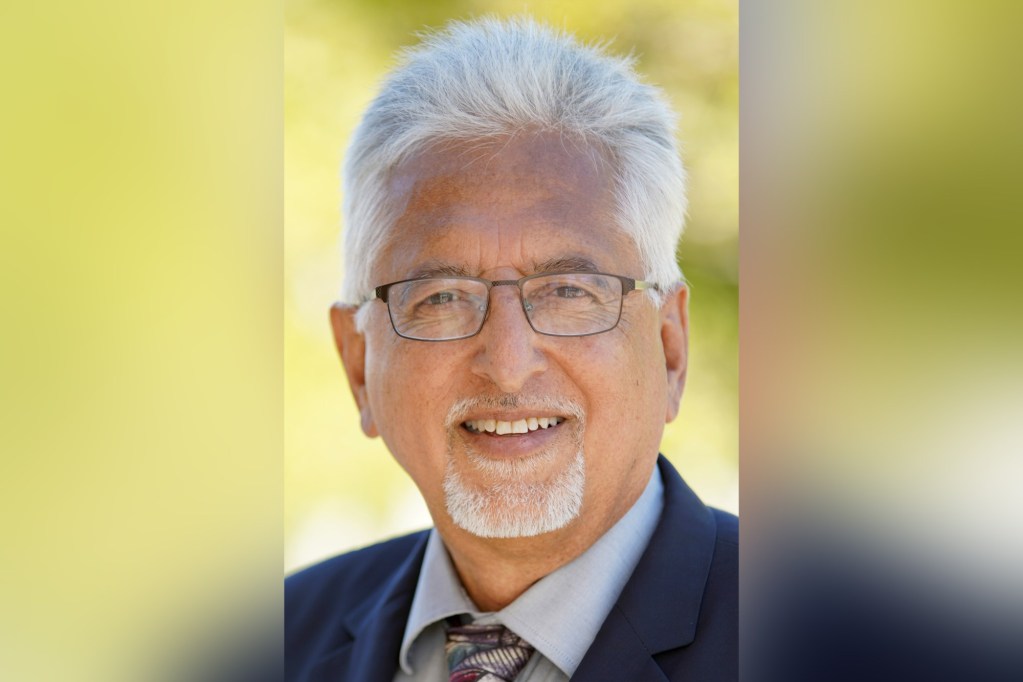
Despite these findings, Dr. Joseph Wu, director of the Stanford Cardiovascular Institute, reassures the public that mRNA vaccines remain highly safe and effective, having been administered billions of times globally. “The mRNA vaccines have done a tremendous job mitigating the COVID pandemic,” Wu stated, underscoring that the risks associated with COVID-19 far exceed those from the vaccines.
The study specifically notes that myocarditis, an inflammation of the heart muscle, occurs in roughly 1 in 140,000 individuals after the first vaccine dose, escalating to 1 in 32,000 after the second dose. Rates are most pronounced among males under 30, affecting about 1 in 16,750 vaccine recipients. Symptoms typically manifest within one to three days post-vaccination and include chest pain, shortness of breath, and elevated cardiac troponin levels, a marker of heart muscle injury.
While these cases of myocarditis are generally mild and resolve quickly, Wu warns that serious inflammation can lead to hospitalization or severe outcomes in rare instances. He notes that the likelihood of myocarditis from a COVID-19 infection is approximately ten times higher than from mRNA vaccines.
The researchers conducted an in-depth analysis of blood samples from vaccinated individuals, revealing that two specific proteins, CXCL10 and IFN-gamma, are significant contributors to myocarditis. By exposing human immune cells to mRNA vaccines, the team observed heightened levels of cytokines—signaling molecules that coordinate immune responses.
To further explore these findings, the team vaccinated young male mice and noted increased cardiac troponin levels, indicating heart injury, alongside immune cell infiltration into heart tissue. Strategies to block CXCL10 and IFN-gamma showed promising results in reducing this damage.
In an innovative twist, Wu and his team examined the potential protective effects of genistein, a soy-derived compound known for its anti-inflammatory properties. Pre-treatment with genistein significantly reduced heart damage from both mRNA vaccination and cytokine exposure. This discovery could broaden the application of genistein in mitigating inflammatory responses beyond COVID vaccines.
As the implications of this research unfold, Wu emphasizes the necessity of balancing the immune response with the risks associated with excessive cytokine signaling, which could lead to myocarditis-like symptoms. “Your body needs these cytokines to ward off viruses. It’s essential to immune response but can become toxic in large amounts,” he explained.
The Stanford study is backed by several grants from the National Institutes of Health and highlights the ongoing need for comprehensive research into vaccine safety. With the potential for broader applications, Wu’s findings may have significant implications for future vaccine development and public health strategies.
As this story continues to develop, it is crucial for the public to stay informed about vaccine safety and potential side effects. The findings from Stanford serve as a reminder of the importance of scientific research in understanding vaccine impacts and ensuring public health.
Stay tuned for more updates on this important issue.