An international team of researchers has developed a groundbreaking resource to identify individuals at genetic risk for elevated low-density lipoprotein (LDL) cholesterol, often referred to as ‘bad’ cholesterol. This research, led by scientists from the University of Toronto and the University of Pittsburgh School of Medicine, aims to enhance the understanding of genetic factors that contribute to heart disease, a leading cause of death globally.
The team meticulously classified nearly 17,000 missense coding variants of the LDL receptor (LDLR) gene. They also examined the resultant changes in the LDL receptor protein structure and function. This work resulted in detailed maps connecting genetic sequence variations to their functional outcomes, which may enable clinicians to better predict patient risks for heart attacks and strokes.
The authors draw parallels between their findings and the early detection of breast cancer through mutations in the BRCA1 gene. They hope that identifying damaging variants in the LDLR gene will allow for timely preventive measures in patients, even when their LDL levels appear normal. “Even with normal LDL levels, a person might be at an elevated risk of a heart attack due to disease-causing variants in the LDL receptor,” explained Frederick Roth, PhD, who serves as professor and chair of computational and systems biology at the University of Pittsburgh.
Roth is the senior author of the study published in the journal Science, titled “The functional landscape of coding variation in the familial hypercholesterolemia gene LDLR.” The research team conducted an extensive investigation into how these genetic variants affect both the presence of LDL receptors on cell surfaces and their ability to uptake LDL, leading to a comprehensive understanding of their biochemical functions.
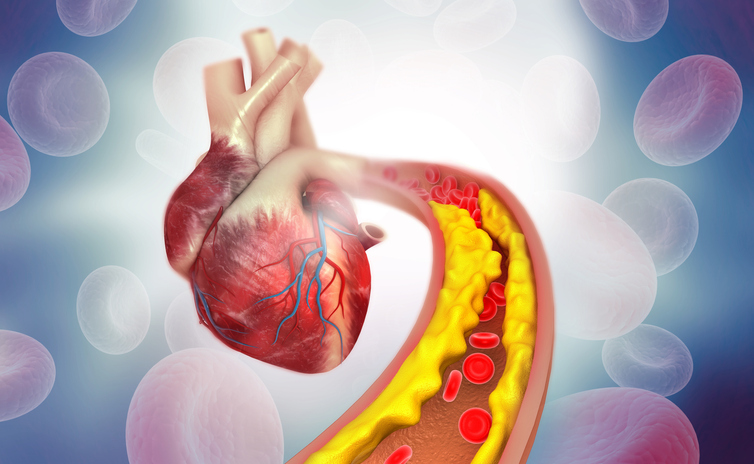
Heart disease remains a significant health crisis, particularly in the United States, where it claims nearly 700,000 lives annually. While lifestyle factors such as diet and exercise contribute to heart disease risk, genetic predisposition plays a crucial role in the development of conditions that lead to plaque accumulation in the arteries. Variants in the LDLR gene are a primary genetic factor driving cardiovascular disease.
The study highlights that heterozygous familial hypercholesterolemia (HeFH), characterized by elevated LDL cholesterol levels, is one of the most common genetic causes of cardiovascular issues. “Genetic variants in LDLR can disrupt the clearance of LDL, accounting for approximately 80% of molecularly diagnosed HeFH cases,” the authors noted.
In healthy individuals, LDL cholesterol functions as a carrier of ‘good’ cholesterol, which is essential for various bodily functions. However, mutations that impair the LDL receptor can lead to dangerously high LDL levels, increasing the risk of heart disease. By identifying pathogenic variants in the LDLR gene, the research team suggests that clinicians can achieve more accurate diagnoses and develop effective treatment plans beyond standard lipid profiling.
Despite advances in gene sequencing technologies that can decode genetic information rapidly, interpreting the vast amounts of data remains a challenge. The team emphasized that many LDLR coding variants lack definitive clinical classifications, limiting timely interventions for patients at risk. “Definitive classifications are lacking for nearly half of clinically encountered LDLR missense variants, limiting interventions that reduce disease burden,” Roth and his colleagues explained.
To address this gap, the researchers classified almost 17,000 variants and assessed their effects on LDL receptor functionality. Their findings produced quantitative insights regarding the efficiency of LDL clearance, equipping healthcare professionals with vital information to manage patients’ risks of elevated LDL levels.
The study emphasizes that functional scores derived from the research correlate with hyperlipidemia phenotypes in human cohorts, providing a robust framework for enhancing the understanding of familial hypercholesterolemia. “These variant impact scores have the potential to increase the number of diagnoses of familial high cholesterol for those with unclassified variants by a factor of ten,” noted Dan Roden, MD, a clinician-scientist at Vanderbilt University Medical Center.
Additionally, the research uncovered a subset of LDL receptor variants whose ability to uptake LDL was inhibited by high levels of very low-density lipoprotein (VLDL). This unexpected finding opens new avenues for further research into the implications of VLDL on LDL uptake and overall human health, as stated by first author Daniel Tabet, PhD, from the University of Toronto.
This initiative is part of a broader effort co-founded by Roth called the Atlas of Variant Effects Alliance. This collaborative project involves over 500 scientists from 50 countries, all committed to mapping the functional effects of genetic variants across various inherited disorders. Through these combined efforts, researchers aim to build comprehensive resources that will facilitate the understanding of gene variants associated with a wide range of diseases, ultimately improving patient care and outcomes.