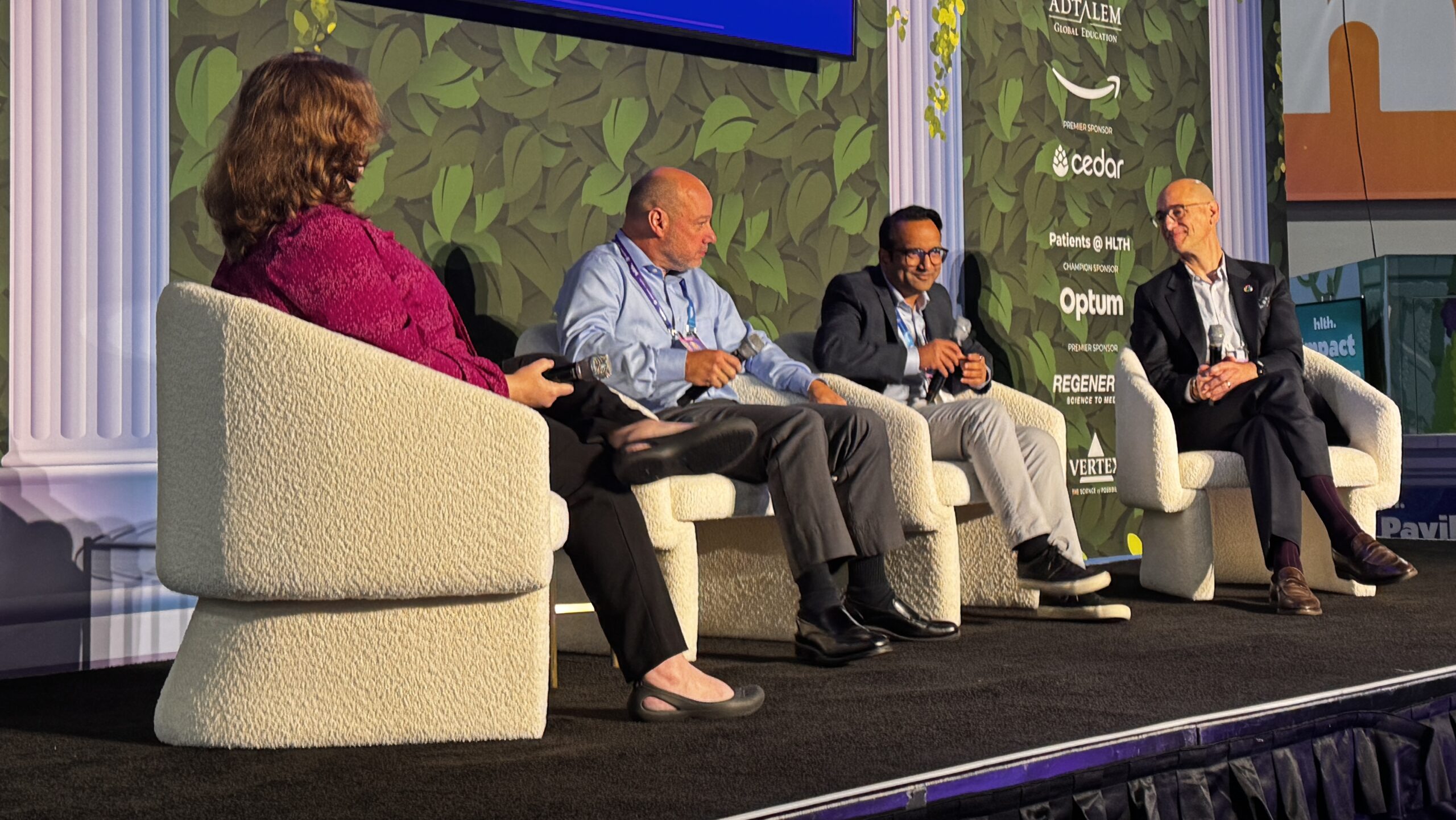
During the HLTH conference held in Las Vegas, Optum, a subsidiary of UnitedHealth Group, introduced a new real-time claims management system called Optum Real. This innovative platform aims to streamline the claims process between healthcare providers and insurance payers, addressing the growing frustration among providers regarding delays and denials from insurers.
The announcement comes at a critical juncture, as provider dissatisfaction has reached unprecedented levels, often attributing the issues to a pervasive “delay and deny” policy by insurers. According to Puneet Maheshwari, Senior Vice President and General Manager of Optum Real, the existing claims process is burdened by a lack of transparency. He stated, “If I have to summarize it in one word, I would say the biggest challenge in claims and reimbursement is guesswork.”
Optum Real aims to eliminate this guesswork by facilitating real-time data exchange between payers and providers. The platform allows for the identification and resolution of known issues at the point of claim submission, ultimately expediting the reimbursement process. As part of the rollout, UnitedHealthcare has become the first health plan to adopt this technology.
Transforming the Claims Process
The traditional claims process can be cumbersome, often taking two to three weeks for approval. In some cases, it may stretch to months if errors occur. Maheshwari explained the current workflow: documentation is completed by providers post-encounter and sent to various teams in batch mode. This method frequently results in lost information and repeated cycles of resubmissions.
Optum Real seeks to address these inefficiencies by introducing capabilities that enable healthcare providers to receive immediate responses regarding patient coverage and reimbursement details. For instance, when a patient arrives for an MRI, the provider can instantly verify coverage and associated costs, significantly reducing administrative overhead.
Maheshwari elaborated, “What real-time transparency enables is that it removes the guesswork. Real transformation comes when you can ask these real-time queries in the moment of care that really matters.” This capability allows providers to address the complexity of patient cases while ensuring the accuracy of documentation and coding.
Challenging the Status Quo
While the optimism surrounding Optum Real is palpable, some skepticism remains regarding the feasibility of a truly real-time system in the healthcare landscape. Critics argue that transparency has historically been lacking, with payers often reluctant to share essential information. Maheshwari acknowledges this challenge, noting that previous solutions have focused on enhancing AI capabilities separately for payers and providers, leading to continued inefficiencies.
He asserts that the key to success lies in fostering real-time transparency, which has been made possible through the opening of APIs by UnitedHealthcare. This initiative promises to provide detailed information regarding patient eligibility and benefits, thus bridging the gap that has long existed between providers and payers.
Statistical data reveals that approximately **80%** of claims are approved upon first submission, but a notable percentage—between **10% to 20%**—require reworking due to insufficient information or errors. Maheshwari points out that the majority of administrative overhead stems from this rework, rather than genuine medical necessity denials, which remain in the low single digits.
The healthcare industry currently spends an estimated **$300 billion to $350 billion** on revenue cycle management (RCM) and payment integrity efforts, a significant amount that could be reduced through the efficiencies introduced by Optum Real.
As providers across the nation contemplate the potential benefits of this new system, the outcomes remain to be seen. Notably, Allina Health, a Minnesota-based health system, has reported substantial savings since implementing Optum Real. As the system gains traction, it is hoped that the era of “delay and deny” tactics employed by insurers will be significantly diminished.
The healthcare community is encouraged to share their experiences with the UnitedHealthcare claims process in light of these developments. Optum’s initiative represents a pivotal step toward transforming the reimbursement landscape, but only time will reveal its effectiveness in practice.