Patients across the United States are increasingly facing hurdles in accessing necessary medical care, often due to complications with insurance coverage. Traci Hurley recounts the distressing experience of watching her husband, Dan Hurley, fight cancer in late 2021. “It was heartbreaking, and it was awful,” she stated. The difficulties were compounded by frequent battles with their insurance provider over coverage for treatments recommended by their physicians. “No family should have to go through having to fight to get treatment while fighting for their lives,” she added.
Many Americans are struggling with high deductibles or experiencing denials for essential tests and treatments. Dan, an ear, nose, and throat surgeon, was well-versed in navigating insurance challenges for his patients, yet he and Traci encountered significant issues while trying to secure care during his battle with chondrosarcoma, a rare bone tumor. Traci noted that their insurer denied many treatments, including essential scans and medications, on the grounds that they were “not medically indicated.”
Insurance Denials and Financial Incentives
Ron Howrigon, a former health insurance executive turned consultant, highlighted the business dynamics at play. He explained, “Health insurance companies know that five percent of their members account for 50 percent of all the costs. So, I have this huge financial incentive to make their lives as difficult as possible.” This model creates a disincentive for insurers to provide coverage when patients require it most.
Determining the frequency of insurance denials is challenging, as companies are only mandated to report data for plans purchased through healthcare.gov. A CBS News analysis of approximately 1.3 billion health insurance claims from 2024 revealed that insurers denied 19% of in-network claims, equating to about one in five. Notably, United Healthcare, the largest insurer, reported a decline in denials from one-third of its federal claims in previous years to 10% across all its plans this year.
Impact on Patients and Healthcare Providers
Dr. Elisabeth Potter, a surgeon at a Texas surgery center, voiced her frustration regarding insurance companies, stating, “They have, honestly, made it more difficult to be healthy in the United States.” She noted that insurance denials often lead to increased operational costs, as her staff spends considerable time resolving coverage issues.
For instance, Jeannie Lee, a 40-year-old mother diagnosed with breast cancer, faced denial from her insurance for a critical procedure that could have been performed alongside her double mastectomy. This delay heightened her risk of developing lymphedema, a painful condition that can significantly impair arm function. After receiving financial assistance from a non-profit established by Dr. Potter, she was finally able to undergo the procedure.
Dr. Potter frequently finds herself defending her treatment decisions to insurance company medical directors, who often lack specific expertise in her field. This disconnect can lead to absurd situations, as she described in one instance when she received inquiries about a patient’s overnight hospital stay during surgery.
Despite her challenges, Dr. Potter’s commitment to her patients remains unwavering. However, she faced repercussions after posting about an urgent call she received from United Healthcare questioning her medical decisions during surgery. This led to threats of legal action from the insurer, which she interpreted as an attempt to silence her advocacy for patient care.
Appealing Denials and the Need for Change
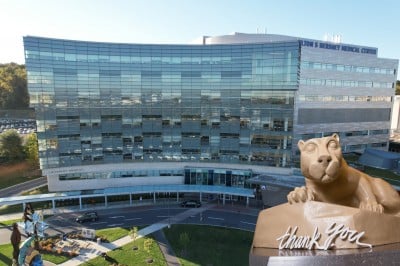
Miranda Yaver, an assistant professor at the University of Pittsburgh, emphasized the systemic issues within the insurance landscape. She pointed out that many patients are unaware they can appeal claim denials, leading to what she describes as “rationing by inconvenience.” “Fewer than one percent of those in-network claim denials result in an appeal,” Yaver explained, despite a success rate of roughly 50% for those who do.
Traci Hurley reflected on her husband’s struggle against both cancer and the insurance system, describing how Dan spent much of his final months battling for necessary care. Tragically, Dan passed away on August 3, 2023, shortly before Traci received a letter from their insurance company demanding $80,000 for a chemotherapy treatment that had been pre-authorized but was later retroactively denied. “It was such a gut punch to get it that day,” she remarked, highlighting the emotional turmoil that often accompanies such financial demands.
In the wake of her husband’s battle, Traci is committed to advocating for changes in the insurance industry. She believes that insurance companies should be held to the same standards as medical professionals, particularly regarding their decisions that impact patient care. “The act of signing that denial is practicing medicine,” Traci argued, advocating for accountability in the insurance sector.
As patients continue to grapple with the complexities of insurance coverage, the need for reform in how healthcare is administered and insured becomes increasingly critical. The stories of individuals like the Hurleys underscore the urgent need for a system that prioritizes patient care over profit.