A groundbreaking study led by researchers at Cornell University has uncovered new insights into how the psychedelic compound psilocybin interacts with the brain, potentially paving the way for innovative treatments for depression. The research, published on December 5, 2023, in the journal Cell, demonstrates how psilocybin weakens negative thought patterns by altering neural pathways.
The study, spearheaded by postdoctoral researcher Quan Jiang and senior author Alex Kwan, Ph.D., employed an unusual combination of psilocybin and a variant of the rabies virus. This unique pairing allowed the researchers to map how psilocybin rewires brain connections. Specifically, the findings revealed that psilocybin diminishes cortico-cortical feedback loops, which are often implicated in negative thought cycles associated with depression.
Kwan’s lab has a history of exploring how psychiatric drugs like psilocybin and ketamine can reshape neurological circuitry, aiming to develop therapeutic options for mental health conditions. Previous studies indicated that psilocybin could significantly alleviate depression symptoms for weeks or even months after a single dose. In 2021, Kwan’s team demonstrated that psilocybin promotes structural plasticity in the brain, rapidly increasing the formation of dendritic spines and synaptic connections.
“Many were enthusiastic about our earlier findings. Psychedelics hold promise as therapeutics, but understanding their mechanisms remains a challenge,” Kwan stated. “This study reveals that the brain rewiring induced by psilocybin has lasting effects.”
Kwan’s current research sought to identify the specific neural circuits involved in this rewiring process. Instead of traditional imaging techniques, the team utilized the rabies virus, engineered by collaborators at the Allen Institute for Brain Science in Seattle. The rabies virus serves as a mapping tool, effectively charting the complex wiring of the brain by transmitting between neurons.
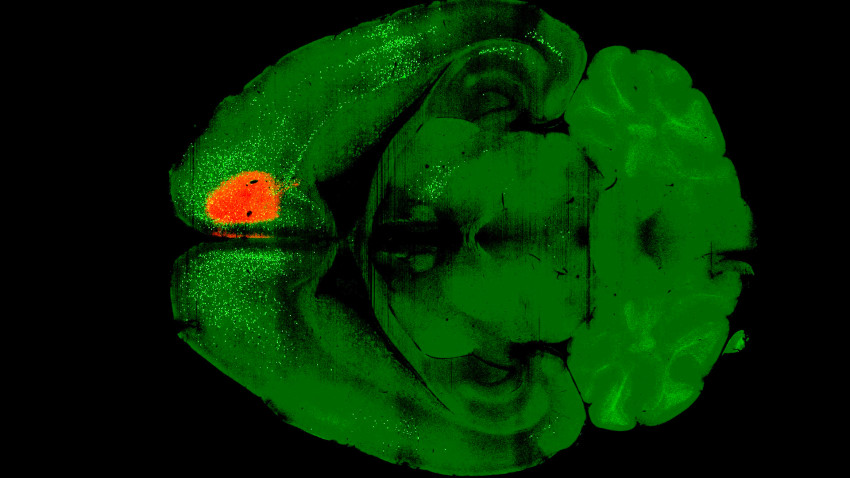
The researchers first administered a dose of psilocybin to the frontal cortical pyramidal neurons of mice. One day later, they introduced the modified rabies virus, which labels connected neurons with fluorescent proteins. After a week, they imaged the brains of the mice and compared them to control subjects that received only the virus. This process revealed that psilocybin significantly weakened recurrent cortical connections, shedding light on why individuals with depression tend to fixate on negative thoughts.
“Rumination is a key factor in depression, where individuals become trapped in a cycle of negative thinking,” Kwan explained. “Our findings suggest that psilocybin may disrupt these feedback loops, allowing for healthier mental processes.”
The researchers also discovered that psilocybin enhances the connections between sensory areas of the brain and subcortical regions, which are essential for turning sensory perceptions into actions. Kwan found this broader impact surprising, as he initially anticipated that the rewiring would be confined to a limited number of brain regions.
“This research offers a comprehensive view of brain-wide changes,” Kwan noted. “Previously, our focus has been on smaller neural circuits.”
Additionally, the study revealed that the level of neural activity in the brain might influence how psilocybin rewires neural circuits. This discovery opens up new avenues for therapeutic interventions, allowing for the potential modulation of negative plasticity while enhancing positive changes.
Co-authors of the study include postdoctoral researcher Ling-Xiao Shao, doctoral student Amelia D. Gilbert, and researchers from various institutions, including Yale University and the Chinese University of Hong Kong. The research received funding from One Mind and the National Institutes of Health.
This innovative approach to understanding the effects of psilocybin on the brain represents a significant step forward in the search for effective treatments for depression, a condition that affects millions worldwide. As research continues in this area, the potential for psilocybin and similar compounds to transform mental health care looks increasingly promising.